Our Work in Northern Canada
Empowering Change, One Innovation at a Time
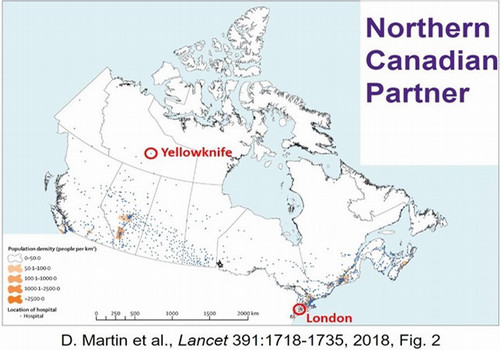
In Northern Canada, unique challenges shape healthcare access. Many communities in Northern Canada are in remote, isolated areas that are difficult to access. These communities have limited healthcare infrastructure, making accessing services challenging and impacting the quality and effectiveness of the care received. Rates of treatable mortality (that is, deaths that should not occur in the presence of timely healthcare) for people residing in the most remote communities are more than 60% greater than the rates for people living in cities with populations greater than 100,000. Those statistics disproportionately affect Canada's Indigenous People, living in some of Canada's most remote communities.
A lack of capacity in Northern Canada's healthcare institutions underlies these healthcare access challenges. Living in an environment of social and economic inequality, education and training rates in Northern Canada suffer (particularly for Indigenous populations). As a result, healthcare institutions are either understaffed or must fill vacancies with short-term/temporary staff from outside the region. The primarily Indigenous residents of small hamlets in the North may not then receive timely, culturally appropriate healthcare and do not fully benefit from economic development opportunities in the region because of lack of community-based expertise.
Travelling long distances for healthcare not only has negative effects on the people of the region, but the region itself. The demand for healthcare (and the need to travel for diagnostics and treatment) contributes to increased emissions and impact on the environment. Bringing health care closer to home for Northern communities ensures accessible, quality and culturally appropriate care while integrating with the principles of planetary health.
To begin to address some of the challenges of health equity, access, and capacity in Northern Canada head-on, Frugal Biomedical Innovations established a collaboration with the Northwest Territories Health and Social Services Authority (NTHSSA).
Frugal Biomedical Innovations will also explore opportunities to support Northern Communities in co-developing professional accreditation programs for individuals (i.e. microcredentialing) to enable more local expertise and technological knowledge in the local health care system.
In 2023, the program announced fifteen Catalyst Grant Award recipients at Western who would receive funding to co-create, develop, test and advance medical innovations that meet patients' needs in remote and low-resource aommunities, including Northern Canada.